Clinically proven to treat stress urinary incontinence
Clinically proven to treat stress urinary incontinence
The Flyte® System treats incontinence by promoting cellular changes to the pelvic floor muscles using transvaginal mechanotherapy. Provide your patients with surgical-level results, without the risks, costs, or recovery time of surgery.

Mechanotherapy, in the form of low-frequency, gentle vibration, is applied directly to the pelvic floor, superimposed on active, guided pelvic floor contractions.
Mechanotherapy has been shown to improve cellular tone and strength and facilitate neuromuscular control and memory.¹
The science

The Flyte wand, made of smooth medical-grade silicone, simply inserts like a tampon. Flyte is comfortable to use and makes it easy to treat incontinence, with a standard treatment protocol of only 5 min per day for 6 weeks.
How it works

Support from Flyte’s on-staff Doctors of Physical Therapy specialized in pelvic health encourages patient compliance and success. Included in the Flyte program, your patients have access to pelvic health education, guidance, and support with setting up and completing their Flyte program.
Meet our clinical experts

In a 2-year follow-up study, participants maintained post-study improved quality of life scores even without continued use of Flyte. 90% of patients say Flyte is simple and easy to use.³
Clinical results
Find out how easy it is to treat stress urinary incontinence with Flyte.
Flyte uses transvaginal mechanotherapy to treat incontinence by strengthening the pelvic floor.
Mechanotherapy is a therapeutic process that triggers the body’s natural repair response and promotes cellular changes to muscle structure and function.¹
Flyte’s intravaginal wand delivers mechanotherapy directly to the pelvic floor.

The wand is designed in size, shape, and resistiveness to be in direct contact with the pelvic floor, providing a gentle pre-stretch to the muscles and connective tissues.
Mechanical stimulation, in the form of low-frequency vibration, is delivered to the pelvic floor muscles.

The resulting microdamage to the pelvic floor muscle cells triggers the body’s natural tissue repair response, increasing muscle fiber recruitment and leading to improved muscle strength and tone.¹
82% of patients were continent in 6 weeks; mean pelvic muscle strength increased by 53%.²
Flyte superimposes mechanotherapy on active, guided pelvic floor contractions. Flyte’s controller and optional App guide your patient through each 5-minute session, providing visual feedback on pelvic floor muscle control.

Flyte begins with an 8-second rest period.

Your patient is cued to inhale and relax their pelvic floor muscles for a 2-second period. Mechanotherapy treatment is delivered.

Your patient is cued to exhale and contract their pelvic floor muscles for a 5-second period. Mechanotherapy treatment is delivered.
These 3 steps repeat 20x in each daily 5-minute session. Urinary continence is achieved in 2-12 weeks.
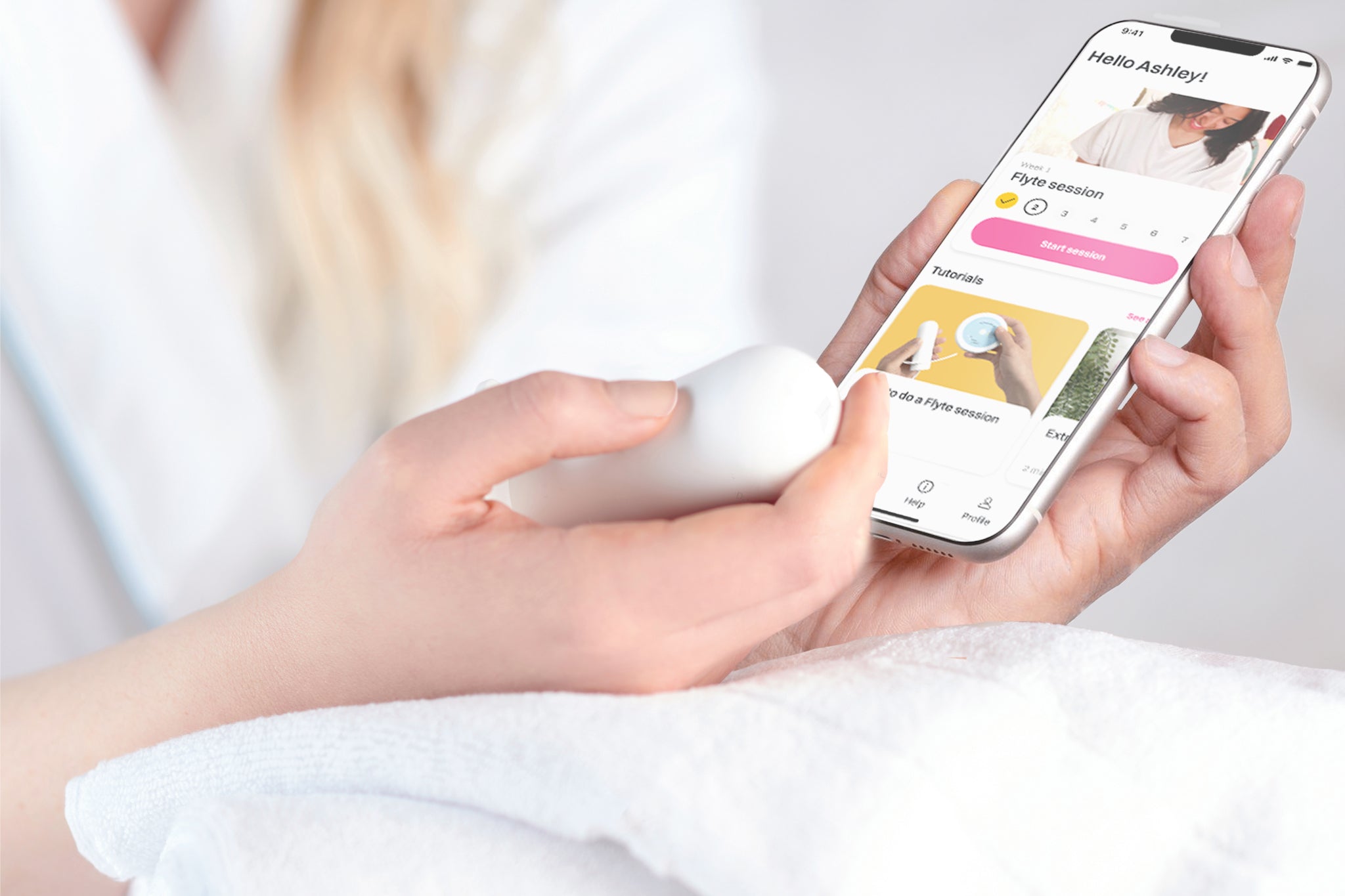
The Flyte App
With a validated incontinence questionnaire taken weekly and the ability to set their own patient-specific goal, your patients are motivated to complete their treatment.
Staying compliant is simple. The Flyte App tracks session completion and weekly progress in incontinence severity score and personal goal. Patients also see a graph of historical pelvic muscle control as measured by the device.
Flyte superimposes mechanotherapy on active guided contractions and relaxations. Real-time visual feedback during each pelvic floor contraction and relaxation helps your patient feel confident and provides insight into growing muscle control.
See how Flyte works, how to prescribe, and how Flyte benefits your patients.